Embry-Riddle Researchers Collaborate to Save Lives of Children with Heart Defects
In a collaboration with the University of Central Florida and the Arnold Palmer Hospital for Children, Embry-Riddle Aeronautical University professor of Mechanical Engineering Dr. Eduardo Divo and Ph.D. student Arka Das are conducting research aimed at saving the lives of children born with only one functioning heart ventricle, a condition that deprives them of crucial blood oxygenation. Without surgery, those suffering from this condition have no chance of survival.
Development of surgical procedures to save these children began about 30 years ago, but the mortality rate is still high, with only about 50 percent reaching age 20. One of the primary challenges to designing effective interventions thus far has been the variability among cases.
“Every case is different from the other,” said Divo. “Some parameters are true for all patients, but the conditions vary widely.”
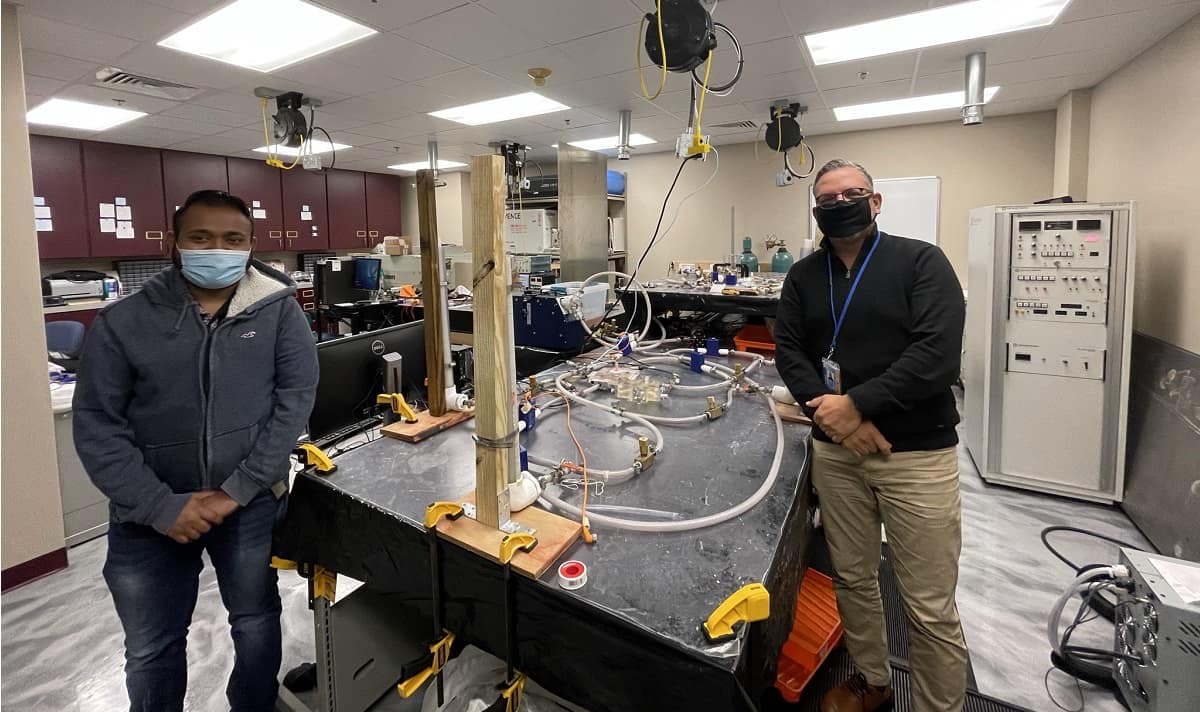
Divo and Das teamed up with Dr. William DeCampli, head of cardio-thoracic surgery at the Heart Institute of the Arnold Palmer Hospital and professor at the University of Central Florida (UCF) College of Medicine, and Dr. Alain Kassab, professor of Mechanical Engineering and director of the Computational Mechanics Lab at UCF. Together, the team will optimize the design of each intervention using computer modeling based on fluid dynamics. Then, they will cross-validate their findings with a benchtop analysis using a mock flow loop, which mechanically imitates the single-ventricle circulation process, developed by Divo and Das.
The mock flow loop “looks like a Rube Goldberg construct,” said DeCampli, “but it enabled us to investigate and confirm some of the predictions arising from our intuition as well as from our computational fluid dynamical studies.”
Their research is supported in part by philanthropy, including a recent grant awarded by Additional Ventures, a nonprofit organization leveraging evidence-based research and subject matter expertise to make an outsized impact.
Divo began collaborating on solving problems related to heart disease about 10 years ago when he was a colleague of Dr. Kassab. DeCampli was looking for a team to work on projects related to cardiovascular disease and recruited Divo. A collaboration began between UCF and the Heart Center at Orlando Health/Arnold Palmer Hospital for Children, and the researchers produced a number of innovations based on computational fluid dynamics that were modifications to cardiovascular surgical procedures.
When Divo came to Embry-Riddle, the collaboration continued, DeCampli said, and Divo “harnessed resources from the rich research environment there to build our program.” Divo also brought in Das to assist with the research.
The collaboration’s latest project is designed to correct a problem encountered in previous surgical interventions in which children with a single-chambered heart undergo a “Fontan Procedure” at about three years old to enable the single functioning ventricle to pump blood to the lungs and to the body. With this procedure, blood returning from the body is routed directly to the lungs rather than passing through the heart first, which requires that the pressure in the body’s veins be increased to drive the blood forward. Unfortunately, this can result in excessive pressure and damage to organs such as the liver and kidneys.
Artificial pumps have been used to assist the blood circulation and allow a lower pressure in the veins, but they require an external energy source, can develop blood clots and may need replacement.
The collaboration’s new design solution uses a device called an Injection Jet Shunt (IJS). It is not a mechanical pump, Divo said, and requires no outside power source, tapping into the single functional ventricle’s own mechanical energy. A model of the device has been presented at engineering and medical conferences and has been tested with computational fluid dynamics and with Embry-Riddle’s benchtop model, optimizing the mechanism to accommodate the specific characteristics of patients. If the model continues to function well in all these test scenarios, it will be used in a human trial, DeCampli said.
“The goal is to improve the quality and length of life in this challenged patient population,” DeCampli said. “This type of project could not be developed without the multidisciplinary teams created by Dr. Kassab, Dr. Divo and myself.”
Divo said the collaboration with DeCampli has been seamless partly because the surgeon is also trained as a physicist. DeCampli holds a degree in physics from MIT and a doctorate in theoretical astrophysics from Harvard.
“We started working with Dr. DeCampli, and it was instant chemistry,” said Divo.
Das, who is due to earn his Ph.D. this spring, said he loves the challenge of this research.
“Research projects with difficult objectives motivate me to perform better at my work,” said Das. “These clinical research projects are more challenging, as the objectives here are not limited engineering achievements but, rather, depend on the clinical outcomes. While conducting these engineering analyses, every step needs to satisfy the clinical requirements, making these projects very challenging.”
For his part, Divo said that being able to provide such bioengineering solutions to help patients in need is extremely motivating.
“That’s one of the reasons I got into bioengineering,” Divo said. “Whatever we do, research-wise, has an immediate social purpose.”

 Michaela Jarvis
Michaela Jarvis